What is a Retinal Detachment?
Share
What is a Retinal Detachment?
A retinal detachment occurs when the retina, a thin layer of tissue lining the back of the eye, separates from its normal position. This detachment disrupts the retina’s ability to process light and send visual signals to the brain, leading to vision impairment or complete loss of sight if left untreated.
This is an emergency, any delay significantly increases the risk of permanent damage to your vision.
If a small hole or tear forms in the retina - this allows vitreous fluid, the gel-like substance filling the eye, to seep beneath the retina. Over time, the accumulation of fluid causes the retina to peel away from the underlying layer.
Symptoms of retinal detachment often include sudden flashes of light, a dramatic increase in floaters, or the appearance of a dark shadow or curtain across the visual field.
Risk factors for developing this condition include age, high myopia (if your eyeglass prescription is over -6.00 diopters), prior eye surgeries, family history, and trauma to the eye.
Understanding the mechanisms and causes of retinal detachment underscores the importance of recognizing early warning signs and seeking medical help to preserve vision effectively.
Early Warning Signs and Symptoms of Retinal Detachment
Retinal detachments often develop suddenly and may not initially cause pain, making it essential to recognize its early warning signs and symptoms.
Early detection can significantly improve the chances of preserving vision and preventing further complications.
- Flashes of Light: Bright flashes, often described as brief bursts or flickers, may appear in the peripheral vision. These flashes can occur sporadically and are most noticeable in dim or dark environments.
- New Floaters: A sudden increase in the number or size of floaters—small, shadowy specks or thread-like shapes drifting across the vision—can indicate a potential issue with the retina. Many patients describe floaters from a retinal detachment as thousands of rust colour dots floating in front of their vision
- Peripheral Vision Loss: The development of a shadow or gray curtain gradually spreading from the edges of vision inward may signal the retina beginning to detach. This symptom typically progresses quickly and requires urgent attention.
- Blurred Vision: Blurriness in central or peripheral vision that doesn't improve with blinking can occur as the retina becomes compromised.
- Reduced Visual Field: The sensation of visual narrowing or an inability to see fine details on the sides may arise in the early stages of detachment.
- Distorted Vision: Images may appear wavy or distorted. Straight lines might seem bent or uneven, especially in the early phase of a detachment.
Who Is at Risk?
Retinal detachment can affect individuals across various demographics, but certain risk factors significantly increase the likelihood of developing the condition. Understanding these risks can help identify individuals who may be more susceptible and warrant closer monitoring by an eye care professional.
- Age is one of the most significant risk factors. Retinal detachment is more common in people aged 40 and older, as the vitreous gel inside the eye naturally shrinks and becomes less stable with age.
- While retinal detachment can affect both men and women, research shows that men may have a slightly higher incidence of the condition.
- Previous eye surgeries, such as cataract removal, increase the risk due to changes in the eye’s natural structure.
- A history of retinal detachment in one eye raises the likelihood of it occurring in the other eye.
- Severe myopia (nearsightedness) has been shown to be a key risk factor because elongated eyes can thin the retina, making it more prone to detachment.
- Blunt or penetrating eye injuries can result in retinal detachment either immediately or as a delayed complication.
- Individuals engaged in high-risk activities, such as contact sports or certain types of manual labor, are more prone to traumatic retinal injuries.
- A family history of retinal detachment can significantly elevate risk, indicating a potential genetic predisposition.
- Certain hereditary conditions, like Stickler syndrome or Marfan syndrome, may contribute to structural defects that heighten risk.
- Diabetic retinopathy, which damages the retina due to blood vessel abnormalities, is a known precursor to retinal detachment.
- Individuals with other retinal diseases, such as lattice degeneration, are considered to be at increased risk.
By recognizing these risk factors, it is possible to take preventive actions and seek prompt care if symptoms develop.
Diagnosing a Retinal Detachment
Retinal detachment is a medical emergency that requires prompt and accurate diagnosis to prevent permanent vision loss. Optometrists and ophthalmologists use a combination of tools and techniques to evaluate retinal health and identify detachment.
Prepare to have the dilating drops when heading to your eye care professional with symptoms of a retinal detachment. It is advisable that you have someone drive you to this appointment. If you live in a rural community, you may have to travel for prompt treatment.
Treatment Options for Retinal Detachment
Retinal detachment is a medical emergency that requires prompt intervention to preserve vision. Treatment options typically depend on the severity, type, and location of the detachment. Most cases must be addressed surgically to reattach the retina and prevent permanent vision loss.
Specialists often tailor the treatment approach to the patient's specific condition. You may need laser treatment that can sometimes be performed in an ophthalmologist's office or you may need more advanced surgical procedures. These can include using a gas bubble to press on the detachment to help the retina stay in place, a scleral buckle that compresses the eye to help with reattachment and in some cases a vitrectomy is needed. In this procedure, the vitreous gel inside the eye is removed and replaced with a gas bubble or silicone oil. This removal allows the surgeon to repair retinal tears and flatten the retina against the back wall of the eye.
Post-Surgery Recovery and Follow-Up
Recovery timelines vary depending on the surgical method and the individual’s healing process. Postoperative care often includes using eye drops to prevent infection and reduce inflammation.
Patients may also need to maintain head positioning as directed, particularly after procedures involving a gas bubble. Regular follow-up visits are essential to monitor healing and ensure complete retinal reattachment.
What Happens If Retinal Detachment Is Left Untreated?
When retinal detachment is left untreated, it can lead to severe and permanent visual impairment. The retina, an essential layer of light-sensitive tissue at the back of the eye, is responsible for sending visual signals to the brain. Once it detaches, the normal functionality of the eye is disrupted, creating progressively debilitating effects. Immediate medical attention is crucial, as the consequences worsen over time.
Gradual Vision Loss
Untreated retinal detachment typically results in the expansion of the detached area. This progression leads to the loss of peripheral vision and further diminishes central vision. As the retina lacks access to its oxygen and nutrient supply in these areas, vision becomes increasingly compromised.
Permanent Blindness
Prolongation of detachment without treatment often culminates in irreversible blindness. The photoreceptor cells of the retina begin to die due to deprivation of essential nutrients supplied by the underlying choroid. Once these cells are destroyed, they cannot regenerate, rendering treatment ineffective in restoring sight.
Preventing Retinal Detachments
Safeguarding eye health is crucial in reducing the likelihood of retinal detachment, a condition that may severely impact vision. While it is not always preventable, taking proactive steps can significantly minimize risk factors associated with this condition.
Schedule Regular Eye Exams
Routine comprehensive eye examinations allow optometrists and ophthalmologists to detect and address early signs of retinal detachment or related complications. Individuals with high-risk factors, such as high myopia or a family history of retinal disorders, should adhere to more frequent screenings as recommended by their eye care professionals. Many retinal holes and tears are found in patients with no symptoms - this allows for prophylactic care prior to vision threatening detachments.
Protect Eyes During Physical Activities
Engaging in contact sports or activities with high physical impact could lead to eye trauma, a risk factor for retinal detachment. Wearing protective eyewear designed for sports or hazardous environments offers an effective way to shield the eyes against injuries.
Monitor Vision for Sudden Changes
Awareness of uncommon changes in vision, such as flashes of light, an increase in floaters, or blurring, is essential. Immediate medical attention sought upon noticing these symptoms can facilitate early intervention, potentially preventing further complications.
Living After Retinal Detachment: Vision Management and Long-Term Care
Living with retinal detachment requires ongoing efforts to manage vision health and prevent complications. Post-treatment care focuses not only on maximizing vision but also on identifying and addressing potential risks of recurrent detachment or associated conditions.
Vision Management Strategies
Patients who have undergone treatment for retinal detachment often experience visual changes that require adaptation. Several strategies can support daily living:
-
Regular Eye Exams: Routine follow-ups with an ophthalmologist are crucial to monitor the healing process and ensure retina stability. Eye exams can also help detect early signs of further detachment or other vision-threatening conditions.
-
Corrective Lenses: Prescribed glasses or contact lenses may help address residual blurriness or visual distortions. In some cases, prism lenses can reduce challenges related to depth perception and alignment.
-
Low Vision Aids: Magnifiers, electronic devices, and high-contrast tools can assist in enhancing functional vision for activities like reading, using electronic devices, or completing intricate tasks.
Lifestyle Adjustments
Adapting daily routines can help patients navigate changes in vision and prevent strain:
-
Lighting: Improved lighting in workspaces and living areas can enhance visual clarity. Adjustable lamps and natural daylight are particularly beneficial.
-
Contrast: Contrast, along with lighting, becomes vital when living with vision loss. Larger print books, e-readers and notebooks with increased contrast are some of the few items that can help.
-
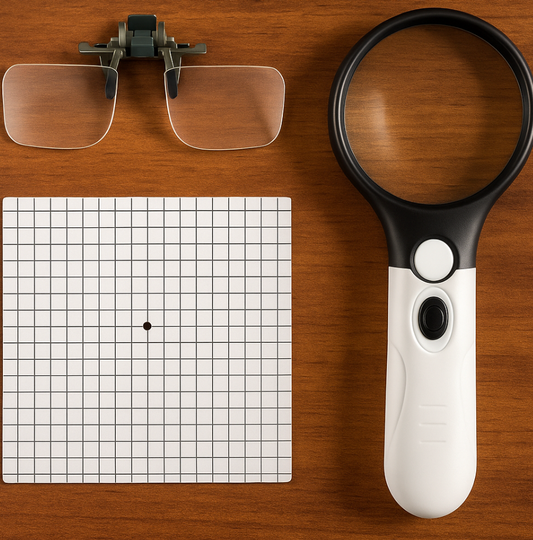
Magnification: You may find yourself needing a magnifier for print that used to be easy to read. We recommend magnifiers that have LED lights to help in lower lighting situations. You can use handheld or stand magnifiers to help. Typically our patients enjoy having a hand magnifier for on the go and stand magnifier at home. Patients also love our 2X flip down magnifier for easy, extra magnification when needed that are compatible with nearly all types of frames.
-
Activity Modification: Limiting physical activities that involve heavy lifting, vigorous motion, or sudden pressure changes is important, particularly in the weeks following surgery.
-
Fall Prevention: Adding non-slip mats and keeping pathways clear can mitigate the risk of falls, often heightened by reduced peripheral vision. Ensuring your home is safe - good LED lighting and anti-slip stair treads are just a few suggestions to help navigate your home with your new level of vision.